Understanding Rating Decisions
After months/years of waiting you finally got your rating decision! The end of the line! But… what the hell does it all mean!?
Ratings decisions are in essence made up of 2 documents:
Narrative (what you get in the mail)
Codesheet (what is kept internally by the VBA)
1. Rating Decision (Narrative)
This document should explain what and how the rater made their decisions.
Rating decision narratives are made up of 5 major sections:
Basic information
Introduction
Decision summaries
Evidence list
Reasons and basis
Basic Information
Your name, file number, and any listed representative.
Decision Summaries
What was granted/denied/deferred, effective dates, and evaluation percentages.
Evidence List
Everything the rater considered in their decision.
IMPORTANT NOTE:
If an important piece of evidence is missing from this list you should strongly consider filing a Higher Level Review (HLR), especially if said piece of evidence would address something the rater noted was missing and is a reason for your denial/under evaluation.
Reasons and Basis
Where the meat and potatoes are stored.
Certain issues like Clear and Unmistakable Errors (CUEs), Traumatic Brain Injuries (TBI), and 1151 denials require long-form decisions. Long-form decisions are when the rater goes into detail and explains ALL the evidence considered, what Element(s) of service-connection were meet and how, what element(s) were not meet, etc.
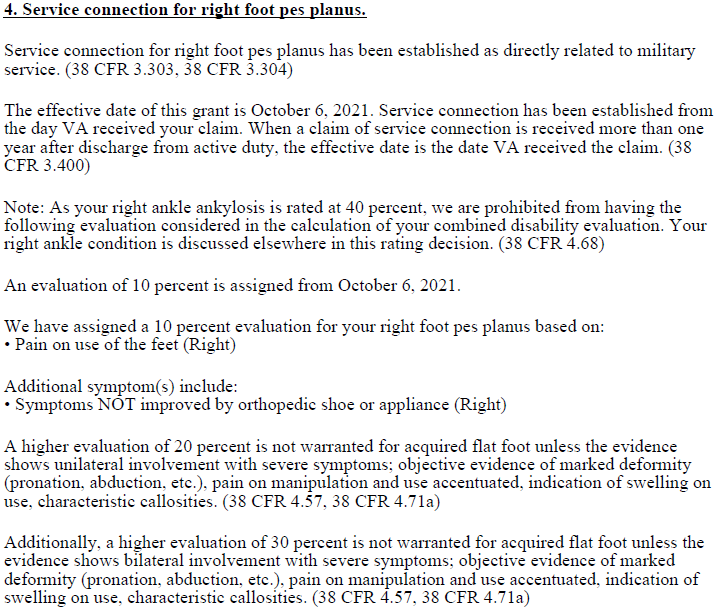
Grants
Short-form grant decisions are broken down into 3 major parts:
Basis of the grant (Direct, Secondary, Presumptive, 1151, Chapter 17)
In the event the effective date is the date VA received the claim or the day after separation, the rater is NOT required to explain how the effective date was determined.
What symptom(s) you have and what your evaluation is because of them.
The requirements for the next higher evaluation.
The rater may also include an additional paragraph explaining how they reached their conclusions, if there is conflicting medical evidence or a decision is particularly complex or confusing.
Denials
Short-form denial decisions are broken down into 3 major parts:
Theories the rater formally considered service-connection under
This typically takes the form of paragraphs of generic canned texts.
Explanation of the decision
Ideally… the rater should include a simple paragraph explaining what you are still lacking in order to get service-connection…however it is not uncommon for a rater too not give a clear explanation in the context of your evidence.
Favorable findings
If you meet one or two of the elements required for service-connection, they will be listed at the bottom.
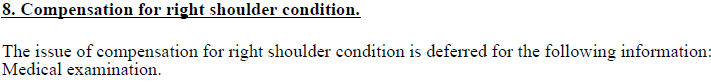
Deferrals
When the rater is unable to make a decision (or fully decide) an issue, they will defer. Most raters will not explain in detail the reason for the deferral. Commonly noting “pending development”.
Generally, when something is deferred it is due to due an issue in the Development process and something needs to be obtained before a rating decision can take place.
Common examples include:
Federal records (medical or otherwise) were not requested;
Private medical records were not requested/require a release;
Medical examinations/opinions were not requested;
Rater requires clarification on a completed examination/opinion;
Medical examination/opinion is missing required information; and
Someone forgot to hit send on an important letter.
2. Rating Decision (Codesheet)
The codesheet is the true backbone 'master record', which contains previous important stuff like grants, denials, current deferrals, current/past combined evaluations, etc. It is also what matters in terms of how Veterans are paid, meaning if the codesheet is wrong but the narrative is 'right', then things are not right! If a narrative is wrong but the codesheet is right, then things will be right for the Veteran - at least administratively.
Codesheets are made up of 6 major sections:
Data tables
Jurisdiction/associated claim(s)
Coded conclusion
Special notion boxes/templates
Signature(s)
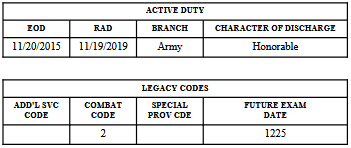
Data Tables
Basic information about your service, who represents you, date of decision, etc.
In the legacy codes box, the only two columns in common use are combat code and the future exam date. With the future exam date meaning that at least one condition has a future Reevaluation and is not considered static.
Combat Codes
IMPORTANT NOTES:
Combat codes have NO impact on evaluations.
It is not uncommon for raters to forget to note things as combat incurred when appropriate.
1 - No conditions are noted as being due to combat
2 - Combat condition(s) are all rated at least 10%
3 - Combat condition(s) are all rated 0%
4 - Mix of combat conditions rated at 0% and over 0%
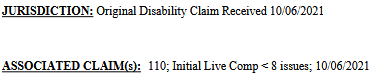
Jurisdiction/Associated claim(s)
Jurisdiction is the reason for the decision (what the decision is deciding), and is largely redundant as it mirrors the associated claim(s). The system does use the selected jurisdiction when it generates the introduction text for the narrative. However, even though a single rating decision can cover multiple jurisdictions the system only allows for one jurisdiction to be selected.
It would be fair to say that between the jurisdiction and associated claim(s), the the associated claim(s) is the more important of the two, since those associated claim(s) show what End Products (EP) the decision is addressing.
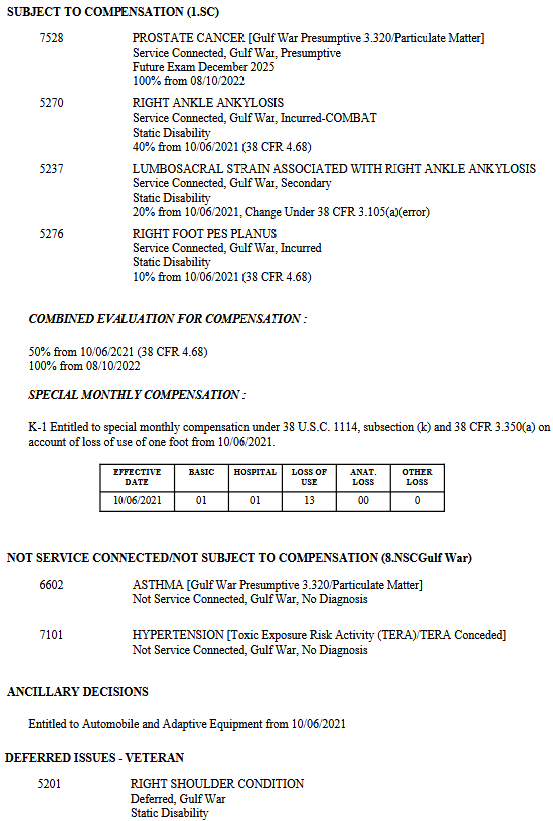
Coded Conclusion
The true heart of the rating decision. Lists out every previous decision as well as the current decision.
Coded conclusions include:
Diagnostic code(s) condition was considered under;
For more information on Diagnostic codes click HERE.
Condition(s) granted service-connection or denied;
[Special issue], identified as text between brackets;
Used to denote special considerations applied in the grant/denial of the condition.
Period of service condition was incurred in or due to (Peacetime, Gulf War, Vietnam, etc);
This is purely for internal VBA bookkeeping.
Basis of grant (incurred (direct)), secondary, presumptive);
If due to combat, to the right of the basis will be “-COMBAT”. This determination has NO impact in how the VA evaluates conditions!
If condition is static or if there is a Routine Future Examination (RFE);
Evaluations and their effective dates;
If the diagnostic code was something else previously it will be shown to the right of the effective date (XXXX).
Historic and current combined evaluation and what conditions have the Bilateral factor applied;
Ancillary decisions; and
Such as Adaptive auto, SAH/SHA, Chapter 35.
Special Monthly Compensation (SMC).
Shows what SMCs have been granted/effective dates, as well as the SMC pay code.
The SMC pay code is the actual driver of the increased pay. Meaning if the rater messes it up, you will be paid incorrectly.
Special Notation Boxes/Templates
There are a total of 4 different special notation boxes/templates that only appear if used:
Clear and Unmistakable Error (CUE) template
Special notation box
Amputation rule template
Accrued grant template
Clear and Unmistakable Error (CUE) Template
Appears at the top of the codesheet, below the data tables. A brief summary of CUEs being called/proposed in the rating decision.
Special Notation Box
Appears towards the bottom of the codesheet. It is commonly used by the rater to ‘speak’ to the POST-VSR, future raters, and those auditing decisions:
Giving instructions to the POST-VSR to invite claims, send letters, etc
Justify and explain why they did something a certain way
Noting the conversion a period of ADT/IADT to AD for disability for disability compensation purposes
Amputation Rule Template
Appears towards the bottom of the codesheet. States which conditions are restricted by the Amputation rule.
Accrued Grant Template
Appears at the top of the codesheet, below the data tables. Denotes a rating decision granting an Accrued benefit.
Signature(s)
This is who made the rating decision. Some decisions will have a second and even third signatures depending on things such as complexity of the decision and/or if the rater is new.
Of course, these signatures are redacted when you request your claim file since… well some of ya’ll get spicy over some unfavorable/bad decisions.
Frequently Asked Questions
-
This is generally done when filing for VA pension to show what evaluation you would have gotten if service-connection was granted.
However, it is most commonly done accidentally when a rater initially plans to grant service-connection and then realizes they cannot for whatever reason, and they forget to go back and remove the evaluation from the system. It is IMPORTANT to realize that this evaluation does NOT itself entitle you to any benefits and does NOT impact your Combined evaluation.
-
Click HERE to obtain.
-
Click HERE for instructions.
Addendums
To see a full example rating decision click the links below:
References
M21-1, Part V, Subpart iv, Chapter 1, Section A - Completing the Rating Decision Narrative
M21-1, Part V, Subpart iv, Chapter 1, Section B - Codesheet Section
M21-1, Part V, Subpart iv, Chapter 1, Section C - Coded Conclusion
M21-1, Part VIII, Subpart iv, Chapter 4, Section A - Special Monthly Compensation (SMC)